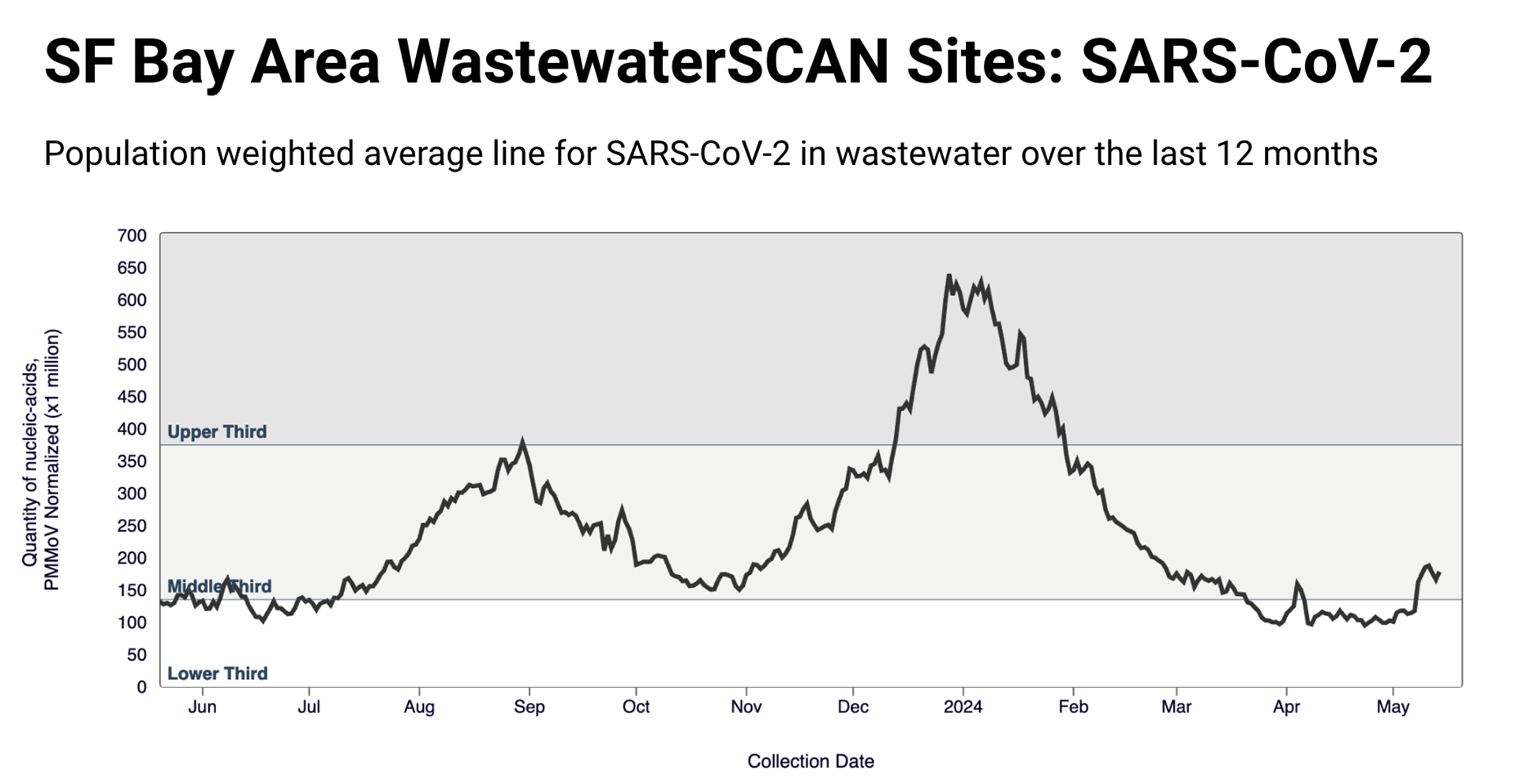
The Bay Area is experiencing a notable rise in COVID-19 levels, detected through wastewater analysis, earlier than last summer. According to Stanford University’s WastewaterSCAN project, COVID-19 levels have increased at 82% of monitored sites across the region. Amanda Bidwell from WastewaterSCAN confirmed that this trend mirrors a national upward trend observed over the past three weeks. The current levels are also higher compared to the same period last year when the summer increase began in late June.
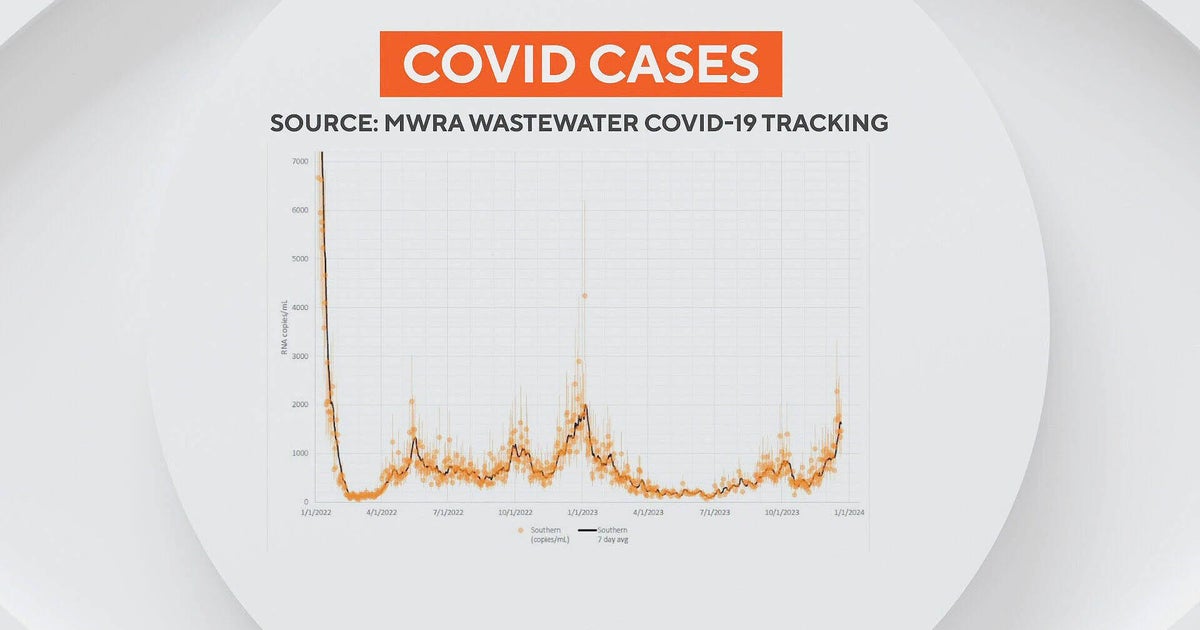
Challenges in Tracking COVID-19
Tracking COVID-19 has become more challenging in 2024. As of May 1, the Centers for Disease Control and Prevention (CDC) no longer requires hospitals to report the number of COVID-19 admissions, reducing a critical data source. Health officials now rely heavily on wastewater data and hospital death statistics to gauge COVID-19 levels. The California Department of Public Health (CDPH) reports a rising seven-day test positivity rate, increasing from 1.9% on April 27 to 3.2% by May 13. However, this data excludes at-home antigen tests, limiting its comprehensiveness.
Trends in Wastewater Covid Illness
Dr. Peter Chin-Hong, an infectious disease expert at UCSF, noted the importance of the wastewater trend, despite uncertainties about the exact number of infected individuals. He suggested that the Bay Area’s earlier summer surge could be attributed to waning immunity, as fewer people are up-to-date on their COVID-19 vaccinations compared to last year. Nationally, only 22% of Americans are vaccinated, with California at 14.4%, leaving many vulnerable to rising infection rates.
New Variants and Community Impact
New COVID-19 variants, informally called “FLiRT” (KP.1.1 and KP.2), are contributing to the rise in cases. While KP.2 has become the dominant strain nationwide, the Bay Area still sees JN.1 as the most detected variant in local wastewater. However, KP.1.1 and KP.2 are gaining prominence in the western states and are expected to increase in transmissibility. Although most people will not become severely ill with these new variants, high-risk groups remain vulnerable. The CDC has stated that there are no indications that KP.2 causes more severe illness than other strains. Dr. Chin-Hong emphasized the importance of available tools to reduce COVID-19 spread and treat infections. He predicted that the reformulated seasonal COVID-19 vaccine, likely to be offered later this year, will be based on the FLiRT variants.
Protecting High-Risk Groups
While the general population may fare well due to previous exposure, high-risk groups, including older adults, immunocompromised individuals, and those with low vaccination rates, remain at greater risk. Low vaccination rates among people aged 65 and older are particularly concerning, despite the availability of an extra vaccine dose for this age group since February. During rising COVID-19 levels, it is advisable to take precautions, such as wearing N95 masks in crowded indoor spaces and ensuring good ventilation when hosting gatherings. High-risk individuals should be especially vigilant. Additionally, upcoming travel plans may warrant extra caution to avoid disruptions caused by COVID-19 infections.
COVID-19 Symptoms and Testing
COVID-19 symptoms in 2024 remain consistent with previous variants, including fever, chills, cough, shortness of breath, fatigue, muscle aches, headache, loss of taste or smell, sore throat, congestion, and gastrointestinal symptoms. Testing remains crucial, especially if symptoms persist. If an initial test is negative, it is recommended to test again within 48 hours.
For those testing positive, the CDC’s updated isolation guidelines allow returning to regular activities once symptoms improve and fever subsides for at least 24 hours without medication. The antiviral treatment Paxlovid remains available by prescription in California. By staying informed and taking appropriate precautions, individuals can help protect themselves and their communities from rising COVID-19 levels.
