In a significant development, up to $4 billion in medical debt accumulated by approximately 2 million North Carolinians over the past decade could be erased. This debt relief initiative is part of a broader effort by the U.S. Centers for Medicare and Medicaid Services (CMS) and the North Carolina Department of Health and Human Services (NCDHHS). The debt relief proposal, approved last year by state lawmakers, will be executed through the Healthcare Access and Stabilization Program (HASP).
Enhanced Medicaid Reimbursement Payments
The NCDHHS will oversee the implementation of enhanced Medicaid reimbursement payments through HASP. The program aims to provide financial relief to hospitals and health systems that agree to participate in the medical debt relief initiative. The North Carolina Healthcare Association (NCHA), representing individual and multi-hospital health systems, played a crucial role in advocating for Medicaid expansion and shaping the legislation that led to this initiative.
Approval and Implementation
The debt relief proposal received positive feedback from state officials and healthcare organizations. State Treasurer Dale Folwell expressed his approval when the initiative was announced on July 1. The NCHA, which has been a long-time advocate for Medicaid expansion, stated its commitment to working with partners to support sustainable solutions for the state’s healthcare system.
The program is approved for fiscal years 2024 and 2025, allowing for additional federal funds to be directed to hospitals to cover the non-federal share of Medicaid expansion costs. Hospitals that choose to participate in the program will receive higher levels of reimbursement in exchange for relieving medical debt for Medicaid enrollees dating back to 2014.
Conditions for Participation
Hospitals must agree to a medical debt and charity care policy developed by the NCDHHS to receive the full amount of authorized funds. This requirement ensures that hospitals provide financial relief to those burdened by medical debt, thereby supporting the state’s healthcare safety net.
The initiative also provides debt relief for individuals not enrolled in Medicaid but who meet certain income criteria or have medical debt exceeding 5% of their annual income. Hospitals participating in the program will receive higher reimbursement rates for providing this relief.
Political and Social Implications
Medicaid expansion in North Carolina has been a contentious issue, with Republicans in the General Assembly historically opposing it. However, last year, the expansion was tied to the state budget, a move that helped secure its implementation on December 1.
Dr. Kody Kinsley, Secretary of the NCDHHS, highlighted the importance of addressing medical debt, stating, “Many people struggle with the burden of medical debt, which can cause them to hold off on getting the essential health care and services they need.”
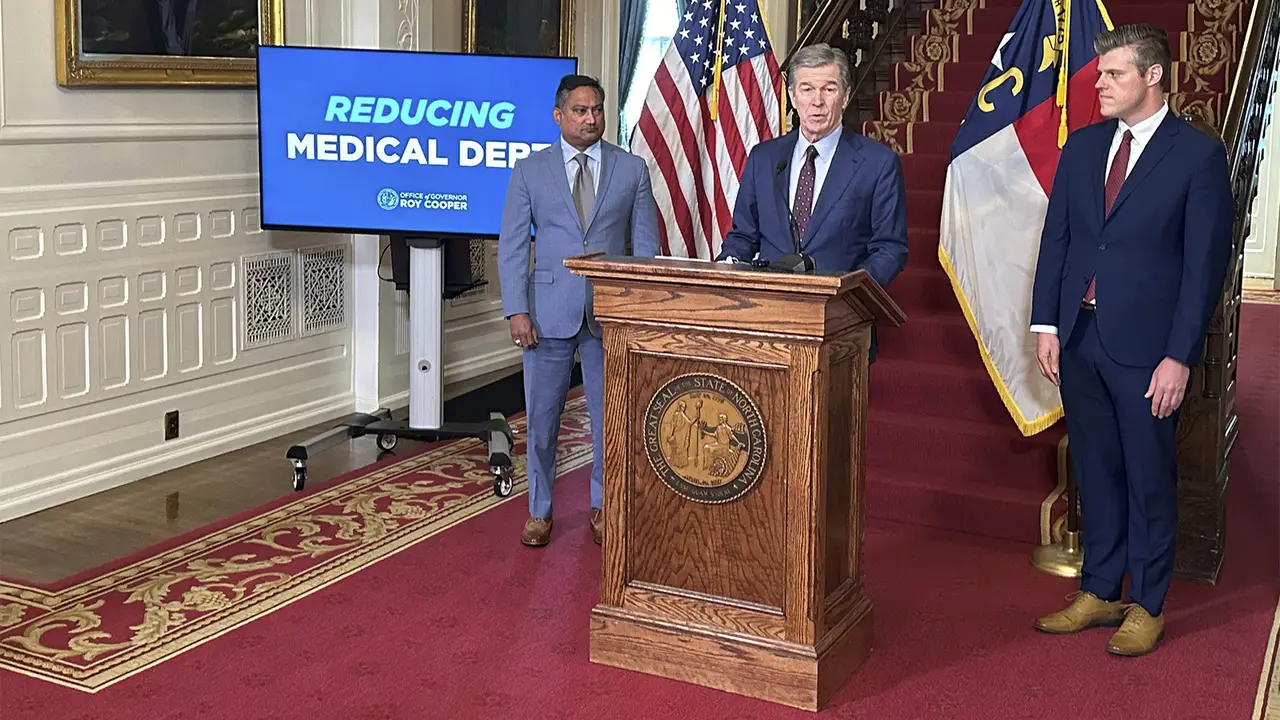
Governor Roy Cooper emphasized that medical debt is often unavoidable, as people do not choose to become seriously ill or have accidents. He noted that the inability to pay medical bills can lead to ruined credit and even bankruptcy, underscoring the need for this relief initiative.
Hospital Participation and Future Outlook
Hospitals have the option to participate in the program. Those that decline will continue to receive Medicaid reimbursement at the base level under HASP. State Treasurer Folwell, who recently ran unsuccessfully in the Republican primary for governor, praised the initiative as a “pro-family” measure and urged Governor Cooper to convince the hospital association to drop its opposition to “pro-consumer legislation.”
The medical debt relief initiative represents a significant step towards alleviating financial burdens for millions of North Carolinians. By providing enhanced Medicaid reimbursement and incentivizing hospitals to offer debt relief, the program aims to improve access to healthcare and support the state’s healthcare safety net. As the program is implemented over the next two years, it will be closely monitored to assess its impact on both healthcare providers and patients.